17 Symptoms and Treatments of Candida Overgrowth
In this article, you’ll learn and discover the 17 symptoms of candida overgrowth, plus how to get rid of it.
Table of Contents
- What are Yeast Infections (Candida)?
- Causes of Yeast Infections (Candida)
- Symptoms
- Natural Remedies for Yeast Infections (Candida)
- Improvement in symptoms is usually noticed after two to four weeks.
- Beneficial bacteria also help to restore the microbial balance within the digestive tract.
- Diet
- List of Foods to Avoid
- Foods Containing Gluten
- List of Foods to Avoid
- Foods Containing…
- Environmental/Lifestyle
What are Yeast Infections (Candida)?
Causes of Yeast Infections (Candida)
- Use of oral contraceptives
- Steroids
- Antacids
- Anti-ulcer medications
- Frequent or long-term use of antibiotics
- High-sugar diets
- Pregnancy
- Diabetes
Symptoms
- Tired or lethargic
- Poor memory
- Feel drained, depleted, or exhausted
- Numbness, burning, tingling
- Stomach pain
- Joint pain or swelling
- Muscle aching or weakness
- Constipation, diarrhea, bloating, gas, or belching
- Bothersome or persistent vaginal itching, burning, or discharge
- Prostatitis
- Erectile dysfunction
- Loss of sexual desire
- Endometriosis or infertility
- Menstrual irregularity or cramping
- Anxiety attacks or crying
- Cold hands and feet feel chilly
- Irritable or shaking when hungry
Natural Remedies for Yeast Infections (Candida)
Coconut Oil
You can treat a yeast infection by applying coconut oil straight from the jar to the affected area. You can rub the coconut oil into the skin or skin fold where the yeast infection is.
Tip: When purchasing coconut oil, be sure to select an organic, pure coconut oil. Some brands may try to pass off a coconut oil blend that won’t get you the same results, so look for 100 percent coconut oil. Pure coconut oil typically won’t have a strong coconut smell.
Milk thistle (Silybum marianum)
This supplement promotes detoxification support. Since milk thistle works on the liver, it can interact with various medications. People with a history of hormone-related conditions or who are at risk for such conditions should speak to their doctors before using milk thistle.
A multivitamin daily
Containing the antioxidant vitamins A, C, E, the B-complex vitamins and trace minerals, such as magnesium, calcium, zinc, and selenium.
Omega-3 fatty acids – (fish oil)
It helps to decrease inflammation and help with immunity. Cold-water fish, such as salmon or halibut, are good sources. Fish oil supplements can increase the effects of certain blood-thinning medications.
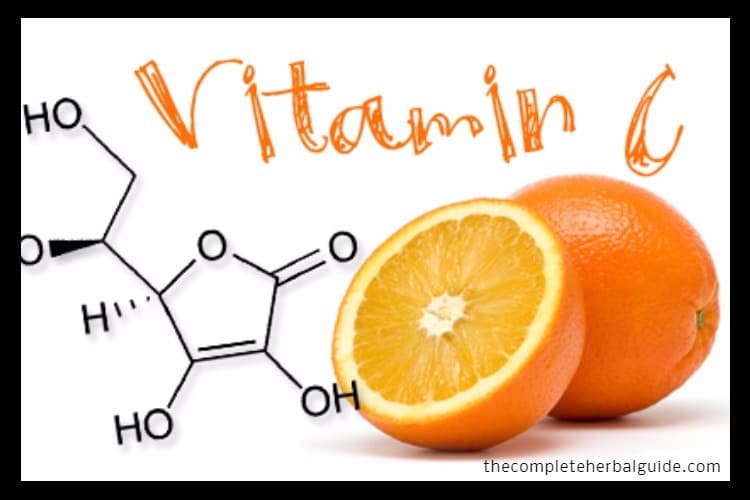
Vitamin C
Vitamin C helps to boost adrenal glands and it is an antioxidant that helps restore the immune system. It also protects the vaginal lining. Vitamin C helps to boost adrenal glands and helps to restore your immune system.
Zinc
Miconazole is an antifungal medicine that fights infections caused by fungus. Zincoxide is a mineral that acts as a skin protectant.
Probiotic supplement (containing Lactobacillus acidophilus)
Probiotics supplements work by populating the intestines with beneficial organisms that can prevent the yeast from overgrowing and help the body to naturally balance the infection.
Grapefruit seed extract (Citrus paradisi)
It’s recommended for its antibacterial, antifungal, and antiviral properties. Grapefruit seed extract can potentially interfere with a variety of medications.
Improvement in symptoms is usually noticed after two to four weeks.
Acidophilus
Beneficial bacteria also help to restore the microbial balance within the digestive tract.
Fiber
Enteric-coated essential oils
Enteric-coated garlic
Diet
Diet is an essential part of the Candida cleanse. The length of time on the Candida cleanse depends on the length of time one has had symptoms, symptom severity, and overall health. People may notice improvement after strict adherence to the diet for two to four weeks. For others it takes months. Once symptoms are gone and lab tests show significant improvement, foods from the restricted list can be slowly incorporated back into the diet.
List of Foods to Avoid
- Sugar – refined sugar is thought to encourage the growth of Candida yeast.
- Honey
- Maple syrup
- Corn syrup
- Maple sugar
- Molasses
- Date sugar
- Turbinado
- Raw sugar
- Demerara
- Amasake
- Rice syrup
- Sorghum
Fruit
Yeast
Foods Containing Gluten
Gluten-containing foods include wheat, barley, and rye.
This includes products made with these ingredients such as:
- bread and pasta.
- Vinegar
- White Vinegar
- Red Wine Vinegar
- Apple Cider Vinegar
- Rice Vinegar
- Balsamic Vinegar
- Any Food Made With Vinegage, such as Mayonnaise, Commercial Salad Dressing, Ketchup, Worcestershire Sauce, Steak Sauce, BBQ Sauce, Shrimp Sauce, Soy Sauce, Mustard, Pickles, Pickled Vegetables, Green Olives, Relishes, Horseradish, Mincemeat, and Chili Sauce.
- Mushrooms: They are typically not allowed on Candida diets.
List of Foods to Avoid
- Milk
- Cheese
- Cottage Cheese
- Sour Cream
- Yogurt And Kefir
- Butter
- Ice Cream And Frozen Yogurt
- Wheat
- Pasta
- Bread
- Sweeteners
- Refined Sugar
- Any White Sugar
- Any Brown Sugar
- High-Fructose Corn Syrup
- Evaporated Cane Juice
- Artificial Sweeteners
- Gluten
All gluten-containing
- Grains – including wheat, barley, rye, spelt, triticale, kamut, couscous, bran, and farina
- Soy
- Tofu
- Milk made of Soy
- Yogurt made of Soy
- Soy Sauce
- Soy Protein Powder
- Tempeh
Coffee and Caffeinated Beverages
- Coffee
- Tea
- Soft drinks
Animal Products
- Beef
- Pork
- Veal
- Sausages
- Hot Dogs
- Deli Meats And Cold Cuts
- Shellfish
Condiments
- Ketchup
- Relish
- Soy Sauce
- Teriyaki Sauce
- Non-Dairy Creamers
- Barbecue Or Steak Sauce
- Salad Dressings Not Made With Allowed Ingredients
- Mayonnaise
- Spreads Not Made With The Allowed Ingredients
- Similar Condiments
Foods Containing…
- Yeast
- Alcohol
Food Additives and Preservatives
Environmental/Lifestyle
Resources
ACOG. ACOG Practice Bulletin. Clinical management guidelines for obstetricians-gynecologists, Number 72, May 2006: Vaginitis. Obstet Gynecol. 2006;107(5):1195-1206.
Black M, Ambros-Rudolph CM, Edwards L, Lynch PJ, eds. Obstetric and Gynecologic Dermatology. 3rd ed. Baltimore, MD: Elsevier Mosby; 2008.
Cabrera C, Artacho R, Gimenez R. Beneficial effects of green tea — a review. J Am Coll Nutr. 2006;25(2):79-99.
Cvetnic Z, Vladimir-Knezevic S. Antimicrobial activity of grapefruit seed and pulp ethanolic extract. Acta Pharm. 2004;54(3):243-250.
Delia A, Morgante G, Rago G, Musacchio MC, Petraglia F, De Leo V. Effectiveness of oral administration of Lactobaccillus paracasei subsp. paracasei F19 in association with vaginal suppositories of Lactobacillus acidofilus in the treatment of vaginosis and in the prevention of recurrent vaginitis. Minerva Ginecol. 2006;58(3):227-231.
Edwards L. Dermatologic causes of vaginitis: a clinical review. Dermatol Clin. 2010;28(4):727-735.
Guo HY, Hu XM, Han DD, Wang ZP, Meng L. Lipid peroxidation and antioxidant status in vagina microenvironment of patients with several common vaginitis. Clin Exp Obstet Gynecol. 2013;40(3):331-426.
Heggers JP, Cottingham J, Gussman J, et al. The effectiveness of processed grapefruit-seed extract as an antibacterial agent: II. Mechanism of action and in vitro toxicity. J Altern Complement Med. 2002;8(3):333-340.
Heitzman ME, Neto CC, Winiarz E, Vaisberg AJ, Hammond GB. Ethnobotany, phytochemistry and pharmacology of Uncaria (Rubiaceae). Phytochemistry. 2005;66(1):5-29.
Holloway D. Nursing considerations in patients with vaginitis. Br J Nurs. 2010;19(16):1040-1046.
Lobo RA, Gershenson DM, Lentz GM, Valea FA, eds. Comprehensive Gynecology. 7th ed. Philadelphia, PA: Elsevier; 2017.
LaValle JB, Krinsky DL, Hawkins EB, eds. Natural Therapeutics Pocket Guide. 2nd ed. Hudson, OH:LexiComp; 2002:452-454.
Mohamadi J, Havasian MR, Panahi J, Pakzad I. Antigungal drug resistance pattern of Candida. spp isolated from vaginitis in Ilam-Iran during 2013-2014. Bioinformation. 2015;11(4):203-206.
Nanda N, Michel RG, Kurdgelashvili G, Wendel KA. Trichomoniasis and its treatment. Expert Rev Anti Infect Ther. 2006;4(1):125-135.
Pereira N, Edlind TD, Schlievert PM, Nyirjesy P. Vaginal toxic shock reaction triggering desquamative inflammatory vaginitis. J Low genit Tract Dis. 2013;17(1):88-91.
Powell AM, Gracely E, Nyirjesy P. Non-albicans candida vulvovaginitis: treatment experience at a Tertiary Care Vaginitis Center. J Low genit Tract Dis. 2016;20(1):85-89.
Quan M. Vaginitis: diagnosis and management. Postgrad Med. 2010; 22(7):117-127.
Reid G, Burton J, Hammond JA, Bruce AW. Nucleic acid-based diagnosis of bacterial vaginosis and improved management using probiotic lactobacilli. J Med Food. 2004;7(2):223-228.
Ross SE, Carter B, Lambert S. Seroprevalence of herpes simplex virus-2 infection among women seeking medical care for signs and symptoms of vaginitis. Herpes. 2009;15(3):46-50.
Scnitzler P, Schon K, Reichling J. Antiviral activity of Australian tea tree oil and eucalyptus oil against herpes simplex virus in cell culture. Pharmazie. 2001;56(4):343-347.
Simopoulos AP. Omega-3 fatty acids in inflammation and autoimmune diseases. J Am Coll Nutr. 2002;21(6):495-505.
Sufka KJ, Roach JT, Chambliss WG Jr, et al. Anxiolytic properties of botanical extracts in the chick social separation-stress procedure. Psychopharmacology (Berl). 2001;153(2):219-224.
Tempera G, Abbadessa G, Bonfiglio G, et al. Topical kanamycin: an effective therapeutic option in aerobic vaginitis. J Chemother. 2006;18(4):409-414.
Torres M, Moayedi S. Gynecologic and Other Infections in Pregnancy. Emerg Med Clin North Am. 2012;30(4):869-884.
Van Kessel K, Assefi N, Marrazzo J, Eckert L. Common complementary and alternative therapies for yeast vaginitis and bacterial vaginosis: a systematic review. Obstet Gynecol Surv. 2003;58(5):351-358.
Yoon JH, Baek SJ. Molecular targets of dietary polyphenols with anti-inflammatory properties. Yonsei Med J. 2005;46(5):585-596.
Healthline